September is NICU Awareness Month, and definitely not something I ever thought I would have to care about, but here we are. I wanted to write a little bit about our experience with our son being in the NICU, and this feels like the best opportunity to do so now that this is a part of our story. I want to start with the statement that I realize we were very lucky to be in the position we were in, that we got the “luxury” of just waiting for our baby to get big enough to learn to bottle feed (and to live within 30 minutes of the hospital). I was reminded of this daily when I walked past teeny-tiny micro preemies who were fighting for their lives, or when there were eerie alarms going off and nurses rushing to bedsides. There was this one alarm that was so loud that when it went off, all available nurses ran to that bed, this happened a couple of times and it makes you sick to your stomach. I was also reminded when one of our neighbors had to get transported to OKC because he was too sick to be helped in our hospital and when that next neighbor was there because of her baby girl’s cleft lip and palette.
NICU Facts
- Each year, half a million babies are admitted into the NICU.
- There are not just preemies in the NICU, they also treat full term babies for many health conditions.
- 1 in 10 babies are born prematurely, and 4 out of 10 cases have no known cause. Preterm labor occurs in 12% of all pregnancies.
- PPROM occurs in about 3% of pregnancies, lucky me!
If you don’t know what PPROM is, you can read more about it in Our Birth Story.
- PPROM occurs in about 3% of pregnancies, lucky me!
- Survival rates, vary widely depending on week born, etc. If you are interested, you can look here.
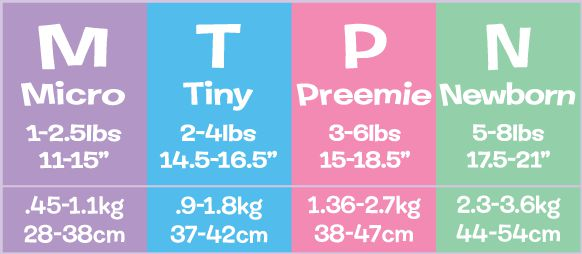
- There are 4 categories of babies in the NICU, see below.
For some reason, when Everett was in the NICU I didn’t do any internet searches or look for any support groups, maybe because I was in denial, or just too busy, I don’t know. I wish now that I would have done a little bit of research. Josh was the main one who told me the few facts we knew, like that he had a pretty good chance of survival and that babies whose parents visited them every day in the NICU have better outcomes. And the NICU nurses told me a little bit about the process, we even had a neonatologist visit us in the hospital room before he was born, but I didn’t know what questions to ask. They gave me a book called “Understanding the NICU” after we discharged, seriously?
Labor and Delivery with a NICU Baby
Having your child admitted into the NICU is a whirlwind and I am still processing it all today. Basically, when you have a baby that they know will be going to the NICU, you have about 500 people (okay, maybe only 10-15 people) in the delivery room, the team for mom and the NICU team. I don’t know how this compares to the delivery room in “normal” situations, but it seems like it’s not normal to have that many people in the delivery room with you. They talked consistently about how long they thought I could have with him before they got him and started working on him. However, they didn’t talk about how they wouldn’t be giving us any updates once they started to work on the baby. I get it, I would much rather them be making sure my baby is okay rather than talking to me about it. But no one gave us a heads up that it doesn’t necessarily mean that something is wrong. Well, I am just assuming that was the modus operandi for a preemie because I wasn’t told that there were any major health issues and his Apgar scores were pretty normal. My situation was a little unique in that I had to go in for emergency surgery, so I didn’t get any updates on him. One of the sweet angel nurses in the operating waiting room offered to get me an update on him for me and they told me right before I went under that he was doing great. I am glad that she offered, because I didn’t ask anyone for updates, I am not sure why though. I don’t think I wanted to know before going into surgery. But I did have a few morbid thoughts prior to surgery that I may never see him again, either because I died during surgery or that he didn’t make it. I thought a lot about something happening to either one of us without knowing his name, since we hadn’t decided at this point. I did a lot of odd things that day, after my surgery was completed, they took me to see him in the NICU, but I mainly wanted to see my husband. And when they showed him to me, he was all hooked to machines and hard to see, so I was not excited to see him. I think I felt responsible for him being in that condition. I was also on a lot of meds, had been in labor for about 12 hours total with minimal sleep, had just given birth, had to be given two liters of donor blood and was coming out of anesthesia. Not to mention we had basically been living in the hospital for 6 days prior to that trying to keep the little booger in there. Therefore, I have forgiven myself for any and all behavior that day, and the days leading up to him being born. I didn’t handle any of it very well.
Being in the hospital for the next 3 days was hard, but one positive was that we could walk downstairs to see him at almost any time. I still felt some serious jealousy pangs when I would hear babies crying in neighboring hospital rooms, or parents walking their newborns around the floor in their adorable little swaddles. I mentioned in my birth story that when you have a baby early that is in the NICU, you don’t really have visitors or congratulations balloons. We didn’t even announce his birth to the world for a few days, mostly because we wanted to know his condition a little better and get some good photos of him. He was in his incubator and initially was hooked up to a CPAP machine, IV fluids, his feeding tube and all of his monitoring stickers for his heart rate, respiration rate, oxygen levels, etc. He was also underneath the UV lights for jaundice. Needless to say, I was unable to hold him until 4 days after he was born. For Dad, that was even later, 7 days after he was born. That was hard for bonding, but I don’t think it stopped us too much, it was hard not to fall in love with this little fighter.





Top left: Baby’s first bath; Top Right: Everett on his side inside his incubator, the nurses moved him all over so his poor little conehead would flatten out evenly; Bottom Left: A picture of the NICU Planning board, they updated his age, length, and weight everyday; Bottom Middle: Super cute photo of his favorite way to sleep; Bottom Right: Our NICU pod and Everett under the UV lights a few days after he was born
Going Home
Leaving the hospital without your baby is really hard, but we were in the hospital for a total of 9 days, and I hadn’t been home at all in that time, so I was ready. But I also knew it would be much harder to get up there to see him. It’s weird having a piece of you somewhere else, I was with him every day for 7 months and then he was out of my body and then just gone most of the time. I could make it okay in my mind at first because we still had to get his nursery ready and have his baby shower, but it quickly gets old. I had enough leave at work to work half days (and I wanted to wait until he came home to take my maternity leave), so my schedule became to wake up, get ready and get to the hospital in the morning for his am feeding time so I could pump for about 20 minutes, do the “hands on” time and then do about 30 minutes to an hour of non-nutritive breastfeeding, which also doubled as skin to skin time before he had to eat and then go get lunch and go home to work until 5. My job was excellent in that they allowed me to telework during this time, I couldn’t imagine having to go into the office everyday during this time. Then, we would have dinner and go back up to the hospital for his 8pm hands-on and feeding time. This would mostly be dad’s time since he left the mornings for just us to bond and breastfeed. He would do most of the work and get to hold him as long as he wanted. This way I was able to get another pumping session in while I was with the baby, which they say is good for your supply. We usually left around 9:30 to get home by 10 and start the cycle all over again.
Everyone asked if we were at the hospital all the time and I felt bad saying no, but we had many talks with our son’s NICU nurses, and the general consensus was that they always tell parents to hold off on taking maternity leave if they can. And that it’s important that the babies stay in their isolette as much as possible and sleep. While it feels weird to leave your baby alone to sleep most of the day, it’s what’s best for the babies. And it helped when they explained to me that he wasn’t supposed to be out of the womb yet, so while skin to skin time is important, it’s just as important for him to be left alone to continue to grow and develop as if he were still in the womb. You could potentially visit almost all day, but I never saw anyone there all the time.
NICU Rules/Procedures:
- Quiet hours were from 2:30-3:30 am/pm and 6-7:30 am/pm. No parents were allowed during this time.
- When you arrived at the hospital you had to follow these procedures:
- Check in with the front desk of the hospital, sometimes you had to wait in line to do this.
- Then, once you got to the NICU you had to pick up a phone and tell them your name and wait for them to buzz you in.
- Once they let you in, you had to wash your hands in their special machines.
- Then we had to give our names, show them our bracelets, and then get our temperature taken.
- Finally, you could go in to the NICU, it’s all open so you can see a lot of the babies, unless the parents were there, then the curtains would be closed in certain sections of the “pods”.
- Everett was in the back of the NICU, so we would walk all the way to the back (this was nice since we seemed to have a bit more privacy and could see out of a window). They usually had the isolettes covered with blankets so it would be dark. He was usually peacefully sleeping and swaddled up. He later learned how to get out of his swaddle, then he could be anywhere in the crib with his feeding tube pulled out.
- Some nurses were okay with you getting started with hands on time as long as you were close to the time to get them out. Some were not though, and we usually had different nurses, so we would just wait for them to show up and tell us we could get him out. Sometimes they were really busy or on break, which was frustrating when you are on a time crunch. Sometimes I would get started regardless. This would make some nurses pretty peeved, but if I have to wait longer than 10 minutes for you to give me the OK when it’s his “hands on” time, then I’m sorry, but I am going to take care of my kid. And this was after I confirmed that it wasn’t detrimental to get started and only a nurse preference issue.
- The normal order for hands-on time is to unswaddle, take their temperature and make sure it was in a normal range and then change the diaper. The nurse wanted to listen to them with the stethoscope and take their blood pressure before you took them out, because this was their time to do their checks as well. Sometimes the nurse preferred to do their part first before you unswaddled them, etc. but it was always different, and we could never seem to do that part right with any of them. It was always hard to find that balance of having the freedom to be their parent while still following all the rules to help make sure your baby was safe and well.
- Then we could hold or do skin-to-skin time, but if you did skin-to-skin they always wanted you to do it for an hour or more. This sounds like a dream, but it’s really hard to do when your baby has tons of cords attached to them, you are in a very small space, are wearing a mask, it’s loud, you’re hungry or have to pee and you can’t do any of those things in there. And you had to have multiple heavy blankets over the baby and a hat that would fall off every 2 minutes to keep him warm. They usually drop their feed at this time, which goes through a tube from a syringe that is held up above their head, so you get the use of gravity. This means that you usually have to hold it, and it can take up to 30 minutes or more for this to empty. That makes an arm quite tired, then you have to wait for the nurse to come cap it off and remove it, you have to keep holding it up or else the milk can come back up into the syringe! And when you do skin-to-skin, you can’t see him since he’s lying on your chest. It definitely has its pros and cons; but it’s hard not to feel guilty when you don’t have the time to do it when the nurses speak its praises constantly about how beneficial it is for both parents and baby.
- It was strongly encouraged to keep them in their isolette/incubator all other times. And they didn’t change their times at all if you had something going on (like your follow up post-discharge appt with your OBGYN). Sometimes they would allow you to push back “hands-on” time by like 15 minutes if you called to warn them. I get it, they can’t be getting behind and their schedules are made so that they can tend to multiple babies and one baby being late can push everyone back. This is just hard for parents.
- Visitors: only Mom and Dad could visit. I am not sure if this was because of Covid or if this is their normal policy. It’s scary to have a baby in there during a pandemic, the thought of one of us getting it and having to quarantine and not see him scared me. It was so weird having this amazing baby to celebrate and not have anyone you love getting to meet him. I started to feel like he wasn’t really real because no one else had seen him in person.
- Tests: The first week he was in the NICU was the most stressful, he had a large battery of tests: they did an ultrasound of his brain to look for any brain bleeds, they took his blood to check his bilirubin levels daily while he was getting UV treatment. I can’t recall but I think they also looked at his blood for a complete blood count (CBC) and glucose, etc.
- Closer to the end of the NICU stay they do an eye and hearing test. It’s scary when they tell you that being premature predisposed him to having sight and hearing loss. Luckily, he passed both of those. He does have some follow up appointments to continue monitoring the development of his hearing and eyesight, because it can also stop developing correctly over time. We just completed the follow up vision screening and he passed! His hearing test keeps getting postponed because he perpetually has fluid on his ears from congestion.
- The day you are planning to discharge, you have to complete the car seat test. They put him in his car seat for 4 hours to see if he could maintain oxygen levels, etc. He passed that the first time as well, luckily!
- Feeding: He was on a feeding tube until about 34 weeks gestation, then they started completing bottle feeds with their physical therapist, Jeff. They started out doing it once a day, then they would gradually increase the # of bottle feeds daily until he got it. They are limited to 30 minutes per feeding, and if he didn’t finish his bottle in 30 minutes, they would consider it a failure and he would get the rest of his feeding through his tube. The reasoning for this was that they would start burning more calories than they were getting when they went past that 30-minute mark. Everett was not a fan of this for a while, I mean why would you want to work hard to eat when the alternative option is just to lay there and have someone pump it right into your stomach? The Physical Therapist was always very positive about him eating, he was just slow and would slow down as he got closer to the end of the bottle. Then once Jeff felt comfortable, he would let his nurses feed him at feedings, and then they finally let us feed him. Some nurses would even mark that he failed with just half an ounce remaining, and some would say it was a win. It was not very consistent, but we did consistently get so-so reports on his eating when he ate during times we weren’t there. They mostly just said he was slow and a little lazy about it, which they said was common for boys.






Top left: Our first family photo!; Top Right: After the first week in the NICU he made a lot of strides, he came off the UV lights, CPAP and his IV; Bottom left: Me holding him for the first time; Bottom left middle: a week or so after he was born when he was just on oxygen; Bottom right middle: Dad holding him for the first time, you can see how they tape the feeding tube to you (this is not high enough and I think we ended up holding it up by hand); Bottom right: Mom and Everett snuggles during skin to skin time.
Discharge
This was the most exciting yet upsetting experience for us. And since telling my story to others I hear it’s pretty common, unfortunately. At the entrance of the NICU there are two hospital rooms that are labeled “Parent Transition Rooms”, when I asked what these were for, our nurse told us that they want some parents to say there overnight with their baby before discharging, but this was only if they were from out of town or couldn’t get up to the hospital daily. Because we were both there at least once a day, I figured we wouldn’t have to do this. Needless to say, I was surprised when they asked me to stay overnight in one of those rooms. Especially because in the week or so leading up to this I had been asking if I needed to start my maternity leave and be up there more often for feedings and I was told I was doing a great job and that we were right on track. I did even stop working the Friday before he was discharged (not knowing when he would be discharged), so I was up there most of the day on Monday when they told me he could be discharged on Tuesday and asked me to stay in the parent transition room with him that night. They did say it was voluntary and I told them that I would if they wanted me to, but that I wanted to go home the next day and give the house a good cleaning and come back up to the hospital in one car. I had a hair appointment scheduled for that next Tuesday afternoon that would take like 30 minutes and I asked if I needed to cancel it and they said no (I know it sounds dumb, this would have been my first haircut since being pregnant, I was afraid of going during Covid while pregnant and while he was in the NICU, but I wanted it done before he came home). The plan was for me to stay overnight with him, then go to my appointment, do a quick cleaning of the house, and come back to the hospital with Josh to pick him up together so he wasn’t in the backseat in his car seat alone. They also had this cute little discharge board we wanted to take a picture with and celebrate with our nurses. Let me add that they didn’t ask Dad to stay the night, just me. He would have stayed, but we decided it would be easier if he were home that night with our dogs.
They put an ankle monitor on him (like I am going to kidnap my own child) and put him in an open-air crib next to the bed, but he was still all hooked up to his monitors and holding him for too long wasn’t really an option unless we wanted to hear alarms go off constantly. Earlier that day he was circumcised after being put in an open-air crib for the previous 12+ hours where he had to suddenly regulate his own body temperature and hear all the sounds in the NICU. This had to affect his sleep, so he was undoubtedly already having a rough time. I am not sure why they do all these huge things at once on their last couple of days there. I wasn’t all that surprised that he wouldn’t finish any feedings with me that evening after everything he went through that day. They also took him in the middle of the night for his crib test, which I am sure also tired him out. While they were doing his crib test, I began to come unraveled because he wasn’t finishing feedings. I didn’t want to have to do this another night and I was nervous about taking him home. It was loud due to the monitors beeping and hearing the main door slam all night long, the bed was sooooo uncomfortable, I couldn’t sleep, and I felt scared and alone with no support on this first night alone with him. I was also upset that if he did get to go home that our first day together at home would be ruined due to me getting no sleep the night before. One of the only benefits about having your baby in the NICU is that you are supposed have enough post-partum recovery time to be on the top of your game when the baby comes home! When his nurse brought him back from his car seat test, I asked her if this was required for him to discharge or if I could just go get some sleep and come pick him up in the morning (since they had previously told me it was voluntary). She didn’t really answer but encouraged me to wait to talk to my doctor who would be there in a couple of hours. When my doctor came to talk to me that morning she asked if I felt comfortable with him going home with us that day, if I felt like he would eat well, and I told her I didn’t know. At this point, even though I wanted him to go home, I was nervous that we would get him home and he wouldn’t eat for us and that he would end up being hospitalized again. She told me she would send the physical therapist, Jeff to come talk to me that morning. When Jeff came, he basically told me he thought Everett would be good to go home, that he has the skills to finish feedings and we won’t have as many rules around feedings at home as he does there and that we wouldn’t be contending with all the stress of the day after all his procedures. He reiterated that we could take breaks at home and he can have snacks in between the 3-hour feedings. This made me feel more confident about him going home.
So, when our nurse asked me again if I felt good about him discharging, I told her that I felt comfortable taking him home that day after talking to Jeff. Then the nurse told me she would talk to the doctor. When she came back, she said the doctor said I had to complete 5 full feedings before he could go home. What? This was a brand new assignment I was never told about before, and I didn’t realize there was some test we had to pass before discharging. I asked to speak to the doctor in person because I was super confused, did they want me to take him home today or not? When the doctor came in, it wasn’t Everett’s assigned physician, it was another one of the neonatologists who I had seen a few times, he was the doctor who came and spoke to us about the NICU while I was in the hospital trying to delay labor. I explained to him my confusion and let him know what the plan for the overnight stay had originally been that everyone had agreed to it and now it seems to be an issue. I also let him know that I didn’t understand why they were acting like I even needed to stay overnight with him when I was there multiple times a day everyday that he was in there. He then started to tell me that they were nervous about him discharging because my doctor and every nurse who had cared for him said he was the most difficult baby they have ever fed. WHAT?!?!?!?!? I responded that I knew it had been a challenge, but every single time I came to the hospital and asked his nurses how feeding went, they all gave good reports. In fact, we were left with the impression that Josh and I were the only ones who didn’t get him to complete his full feedings every time. And we got him to finish feedings quite often. He apologized that this was never communicated to me, but it wasn’t enough, I was pissed. There were SO many opportunities to have this conversation, I saw the doctor nearly every single day and his nurses constantly. I spoke on the phone with the head nurse a couple of times, and I never got any indication that he was this “problem child” that they were now claiming he was.
Josh decided to come up there and help with the feedings after the doctor said it was OK for Dad to help (which is ridiculous that permission for his DAD to feed him was needed). He did great at helping him finish feedings and basically took over so I could go to my appointment and get the house ready for him. I felt bad leaving, but I really needed to get away from the hospital for a little bit, they were making me feel like the worst mother in the world and like I had the most difficult baby. At this point I hadn’t slept in over 24 hours, and I felt attacked, confused and I needed some sense of control. Sometime over the course of the all the back and forth between the nurses, the doctor, Jeff, my husband and I, Everett’s doctor said that I was the one who had to make sure he ate and made some snarky comments like “how will I handle him being home if I can’t do this at the hospital, and that I needed to get used to caring for him on no sleep.” Therefore, I came back and did the next few feedings. He didn’t finish any of them completely, so I was preparing myself to stay there another night and go another 24 hours without sleep. We told the nurses he didn’t finish any of the last few feedings, she went to talk to the doctor, came back and told us he was discharging. Again…WHAT?!??!? Then we were basically rushed out after getting discharge instructions because the shift change was at 6:30 pm and it was almost 6. We didn’t get to celebrate anything or even see his name on the discharge board. We still ended up in a situation where we had two cars there, but we figured it out to leave one car there overnight since it was so late in the day, which wasn’t ideal and just another thing we had to deal with the next day. While we were so happy to get him home, it was clouded in such a crummy and upsetting day and of course we were both leaving worried that we had a super difficult child who wouldn’t eat. Which ended up not happening at all, but I think I was a bit traumatized by this experience because I was so anxious to feed him for such a long time. That eventually went away after he continued to show me what a rockstar he was!
Everett’s First Days At Home






Final Thoughts
The NICU is an amazing place where amazing people do amazing things. I am completely aware that if the NICU didn’t exist that our son would most likely not be here today and that the specific hospital he was in did an excellent job at minimizing any complications he could have experienced. I do think they could do better at parent education and discharge planning. At first, I attributed it to Covid and being short staffed, etc., but anyone I have ever told my experience to that knows anything about the NICU said this happens all the time. Most of our nurses were amazing as well and I know the nurse who was there discharging us was very apologetic over the issues we were having. A NICU stay is an event that is impossible to make a super joyful experience. Knowing that it was going to mostly be a crap time no matter what, makes all of it a little easier to process.
I am sure every woman has their own set of doubts about being a mom, but this was my first time, and quite often in the NICU I felt like I was doing everything wrong. I would dress him, and they would say it wasn’t warm enough and change his clothes. Or they didn’t like the way I held him or something. The nurses had to “overstep” at times to do their jobs according to their policies and procedures. And not being able to establish breastfeeding was hard on me, he was always able to latch and eat, but the whole NICU experience of them being concerned he wouldn’t gain weight ingrained it in me that I always had to know the volume of what he was eating. I also didn’t want to ruin any progress he had made toward bottle feeding . Consequently, I felt like I would be a bad mom if I didn’t exclusively pump. And now I feel like a bad mom because I do exclusively pump – because in the non-NICU world, it’s sort of frowned upon to not actually breastfeed your baby. Looking back now, I probably was taking things a bit too personal in the whole discharge process. I should have just done whatever needed to be done to get him home, but I think I was mostly struggling with worrying whether or not he would be okay to come home. I also wish I would have just gone with the flow a little bit more and handled it better. I WANT to be able to look back on the day he came home with all fond emotions. For now, all the elation is sprinkled with a lot of shame and regret. My husband reminded me then that he is home and is thriving now, and his early birth and NICU stay is just another part of our story and our journey to parenthood. I think of his NICU experience nearly every time I feed him: he gets so excited to eat every time and LOVES his mealtimes so much that he sometimes squeals when it’s time, and I am incredibly thankful.
Do you have a NICU story you would be willing to share? I would love to hear about your experience.